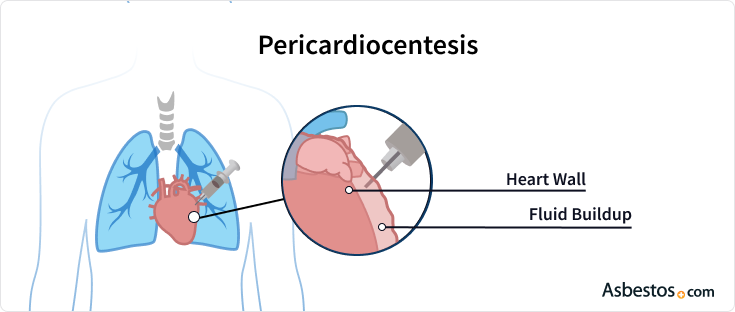
Pericardiocentesis
A pericardiocentesis is a procedure used to treat the buildup of fluid in the pericardium, which is the sac encasing the heart. Sometimes referred to as a pericardial tap, pericardiocentesis can help alleviate symptoms caused by pleural and pericardial mesothelioma.
Written byKaren Selby, RNEdited ByWalter PachecoMedically Reviewed ByDr. Chuong Hoang
Asbestos.com is the nation’smost trustedmesothelioma resource
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
About The Mesothelioma Center at Asbestos.com
- Assisting mesothelioma patients and their loved ones since 2006.
- Helps more than 50% of mesothelioma patients diagnosed annually in the U.S.
- A+ rating from the Better Business Bureau.
- 5-star reviewed mesothelioma and support organization.
Testimonials
"My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family."LashawnMesothelioma patient’s daughter
How to Cite Asbestos.com’s Article
APA
Selby, K. (2023, April 11).Pericardiocentesis.Asbestos.com. Retrieved April 13, 2023, from //www.magnakarsa.com/treatment/surgery/pericardiocentesis/
MLA
Selby, Karen. "Pericardiocentesis."Asbestos.com, 11 Apr 2023, //www.magnakarsa.com/treatment/surgery/pericardiocentesis/.
Chicago
Selby, Karen. "Pericardiocentesis." Asbestos.com. Last modified April 11, 2023. //www.magnakarsa.com/treatment/surgery/pericardiocentesis/.
What is Pericardiocentesis?
The buildup of fluid in the heart lining is known as pericardial effusion. This can cause pressure on the heart leading to dyspnea (shortness of breath) and coughing. The accumulation of too much fluid in the pericardial sac can be very dangerous because it can interfere with the heart working effectively. A pericardiocentesis can effectively remove fluid excess to relieve these symptoms.
Although the way pericardiocentesis is performed has changed over the years, it is actually an old procedure that was introduced in the mid-1800s. By the 1900s, it was the preferred method of treatment for patients suffering from pericardial effusion caused by a variety of disease.
Early procedures carried many risks, but once technology was in place to allow doctors performing the procedure to be guided by ultrasound, it became much safer. Pericardiocentesis is not the only procedure that drains fluid around the heart, but it is generally preferred over invasivesurgery.
Benefits for Mesothelioma Patients
医生建议心包穿刺术过程to mesothelioma patients with pericardial effusion to ease symptoms and improve quality of life. Mesothelioma symptoms, including shortness of breath, coughing and chest pressure, may improve after the procedure. Pericardial effusion can complicate cases of pleural and peritoneal mesothelioma. They can also occur in the very rare primary pericardial mesothelioma cases.
A 2021 case study of a pericardial mesothelioma patient noted that while pericardial effusion was present, the fluid did not contain malignant cells. The study noted that diagnosis for this rare disease is especially difficult because tumor invasion of the myocardium may not appear on radiological imaging.
Although a pericardiocentesis cannot usually lead to a definitive diagnosis of pericardial mesothelioma, it can effectivelytreat symptoms of the cancerand potentially prevent further fluid buildup in the pericardium.
What to Expect from a Pericardiocentesis
Generally, a pericardiocentesis is performed in the hospital, either in a surgical setting, a cardiac catheterization lab or bedside if the patient is already hospitalized. Avoiding eating or drinking for six or more hours prior to the procedure may be requested.
Patients are often set up with an IV in case any medications or fluids are deemed necessary during the procedure.
The anesthesiologist (or other health care worker) then cleans an area below the breastbone and administers a local anesthetic. A long, thin needle is then gently guided into the pericardial sac to draw out fluid. An echocardiogram, which is an ultrasound of the heart, is used to guide the needle and ensure there is no injury to the heart.
Once the needle is correctly in place, it is removed and replaced with a catheter tube. The catheter drains the fluid into containers, sometimes for several hours or possibly overnight.
Some patients feel pressure when the needle enters, and some people may experience chest pain, which is treatable with pain medication. Patients may also benefit from pain medication after the anesthesia wears off.
Recovery from Pericardiocentesis
You should ask your doctor about what to expect after a pericardiocentesis. In general, you should be able to resume normal activities relatively soon after the procedure. However, you should avoid strenuous exercise or physical activity until your doctor says it is OK to do so.
An additional echocardiogram may be used to confirm the absence of fluid reaccumulation. An X-ray may also be ordered to ensure the needle did not puncture your lungs. Your medical team will closely monitor your vital signs such as your heart rate, breathing and blood and oxygen levels.
After leaving the hospital, you should contact your doctor immediately if you experience increased draining from the needle insertion site, chest pain or severe symptoms.
Risks of Pericardiocentesis for Mesothelioma
The patient will be monitored for several hours after the procedure is complete to ensure there are no complications.
Potential problems that can occur during or after pericardiocentesis include:
- A puncture in the heart
- Cardiac arrest
- Abnormal heart rhythms
- Puncturing the liver
- Excess bleeding
- Air in the chest cavity
- Infection around the procedure site
这些并发症很少见,dependin可能会有所不同g on your age, overall health and the severity of the pericardial effusion being treated. The procedure may need to be performed more than once, especially if fluid continues to accumulate in the area.

Recurrent Pericardial Effusion
Several pericardiocentesis procedures may be performed on a patient with recurrent pericardial effusions. A chest X-ray and echocardiography can be used to detect recurring pericardial effusions.
CT scans are sometimes capable of detecting pericardial mesothelioma tumors, though they frequently fail to detect diffuse mesothelioma tumors, which grow in a diffused pattern throughout the pericardium rather than as a solid mass.
诊断测试的液体提取——被称为effusion cytology — is commonly performed after each procedure. Doctors continue using pericardiocentesis for diagnostic purposes. However, the procedure is diagnostic in only 25% of pericardial mesothelioma cases, according to a 2016 study fromHindawi’s Case Reports in Medicine.
Pericardial mesothelioma is rare and difficult to diagnose. Pericardial fluid does not usually contain malignant cells when mesothelioma is present.
In most cases of primary pericardial mesothelioma, confirmation of diagnosis usually requires a biopsy of the tumor. Apericardiectomyis required to obtain a biopsy. This surgery can also relieve pericardial effusion and may prevent recurrence of effusion.










